NextStep
Creators:
Katrine Struve
Fynn Stolt
Curator's Note
Updated: August 2025
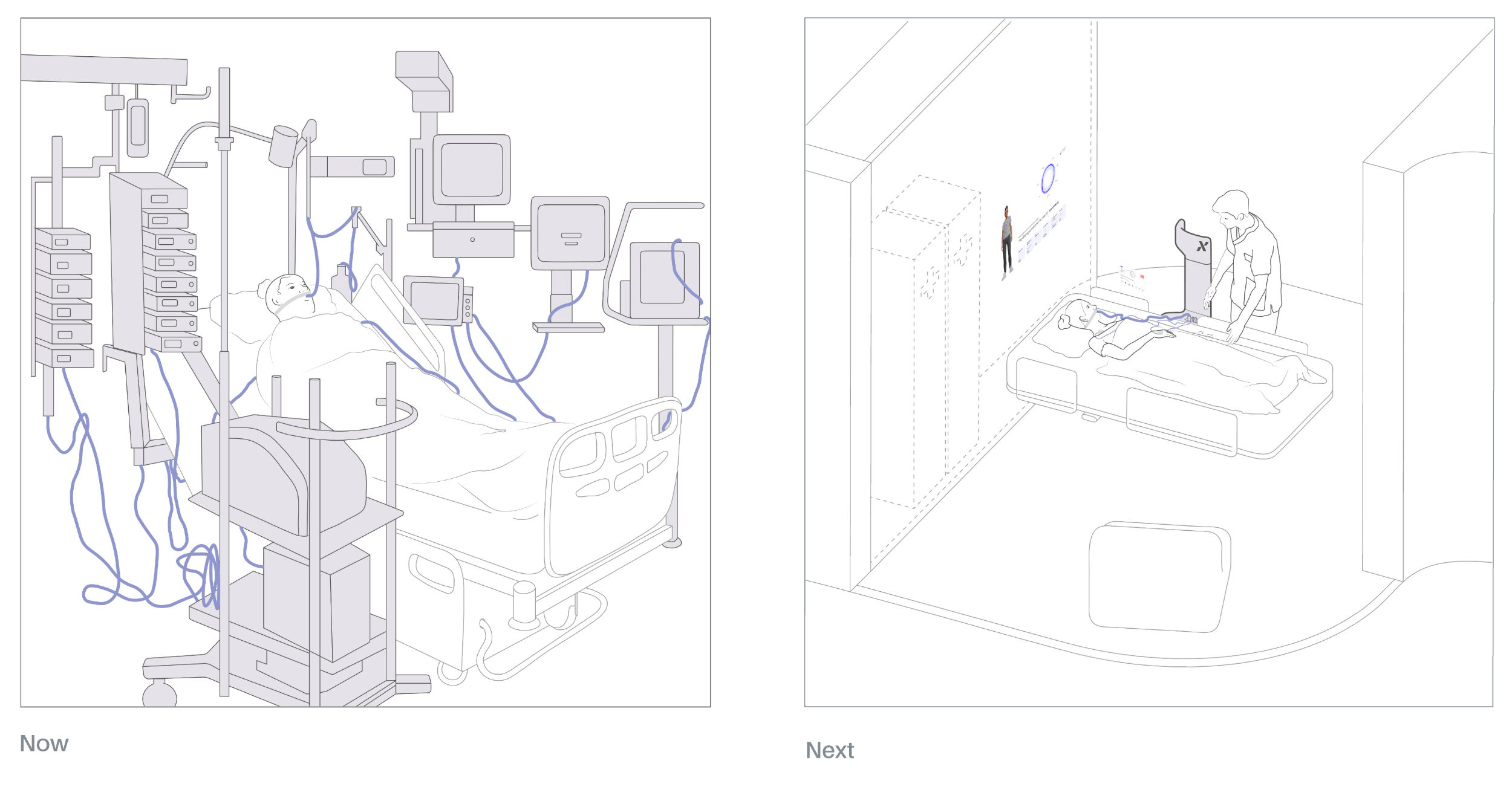
Early mobilization of hospitalized patients decreases ICU‑AW (intensive care unit acquired weakness) by around 40–50 %. Despite strong evidence, early mobilization is inconsistently applied across ICUs. Surveys and reviews show large variation in uptake; adoption is often limited even in high‑resource settings. What if one of the main inhibitors of the early mobilization practices, the lack of dedicated mobility aides and disabling infrastructure, was invalidated? What if technological advances could tackle the problem, almost autonomously?
This project shows an alternative to current ways of caring, that seamlessly blend technology and human care into a desirable design vision.
Abstract
NextStep is a smart system designed to make early mobilization a standard and seamless part of intensive care. Although clinical evidence clearly demonstrates the benefits of early movement—including faster recovery and reduced risks of muscle atrophy, thrombosis, pneumonia, and delirium—it remains under-implemented in daily practice. Contributing factors include cautious risk assessments, high workloads, and limited staffing, all of which hinder consistent patient mobilization.
A well-defined ICU structure facilitates the implementation of early mobilization.
Developed in close collaboration with Dr. Peter Nydahl, a leading nursing scientist at UKSH, NextStep addresses these barriers with an integrated, intelligent solution. Our vision: movement should become as routine as medication in the ICU. Once the patient’s condition allows, bed rest should be limited to nighttime only.

Overview of the Early Mobilization Process
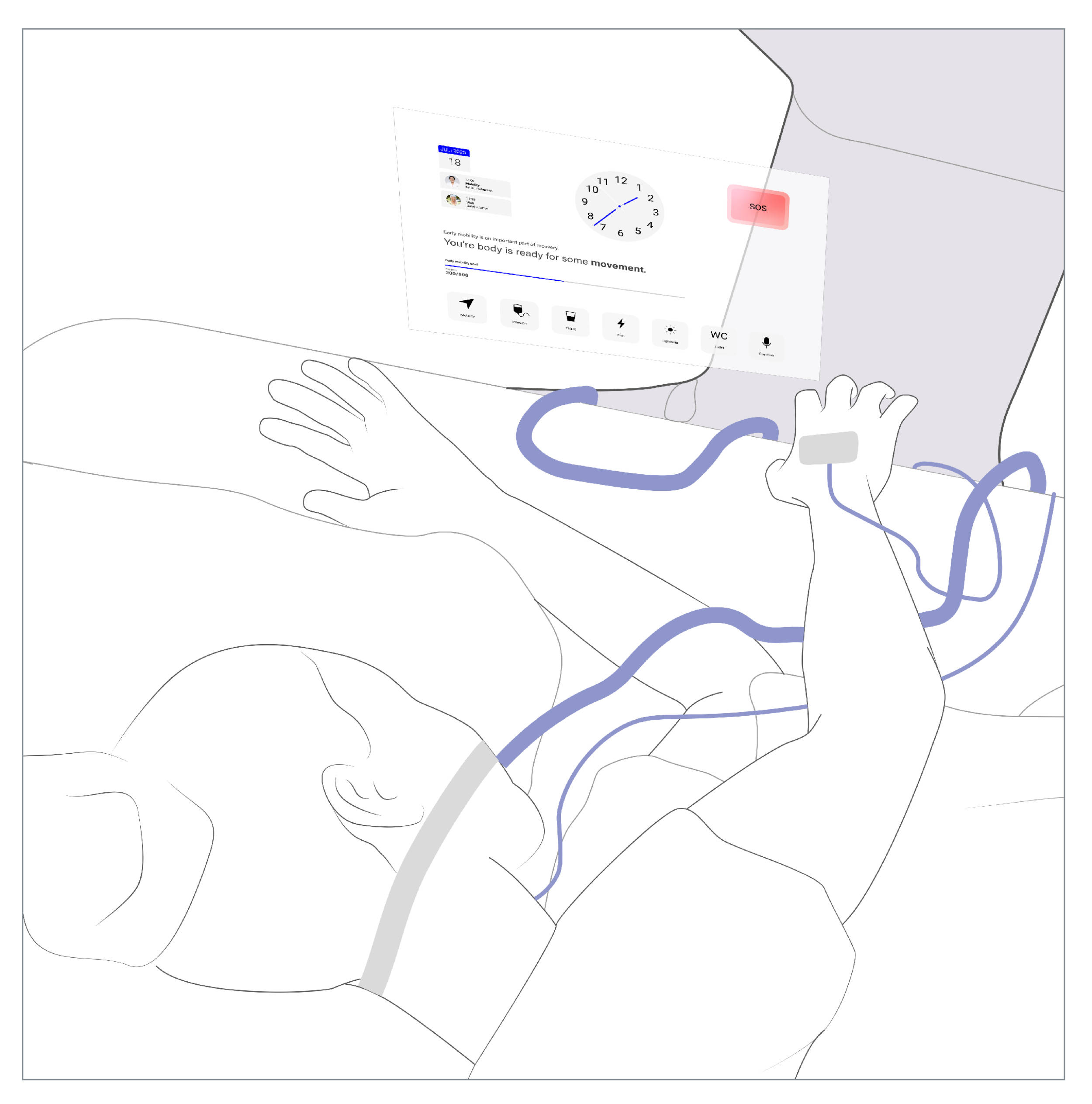
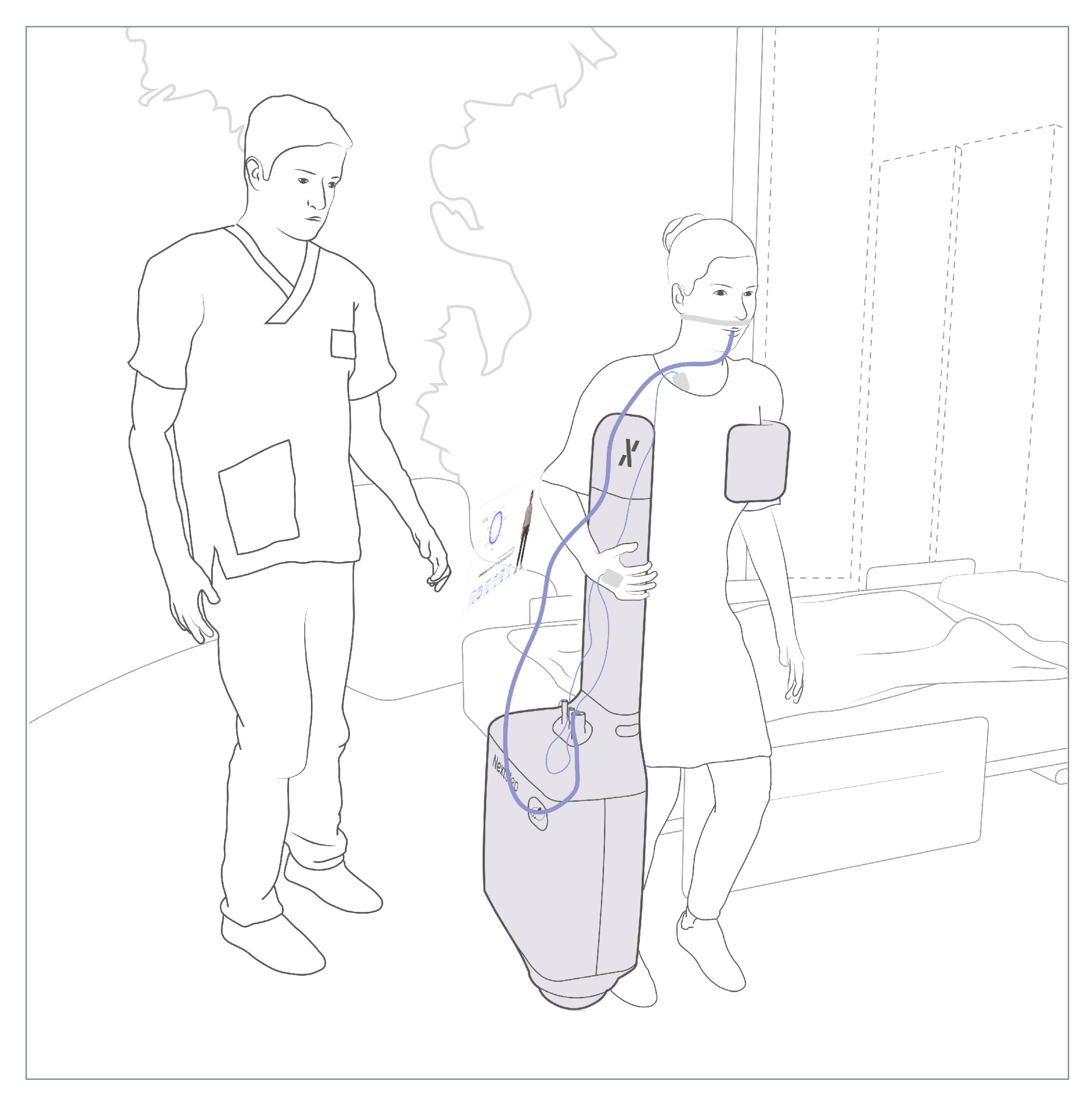
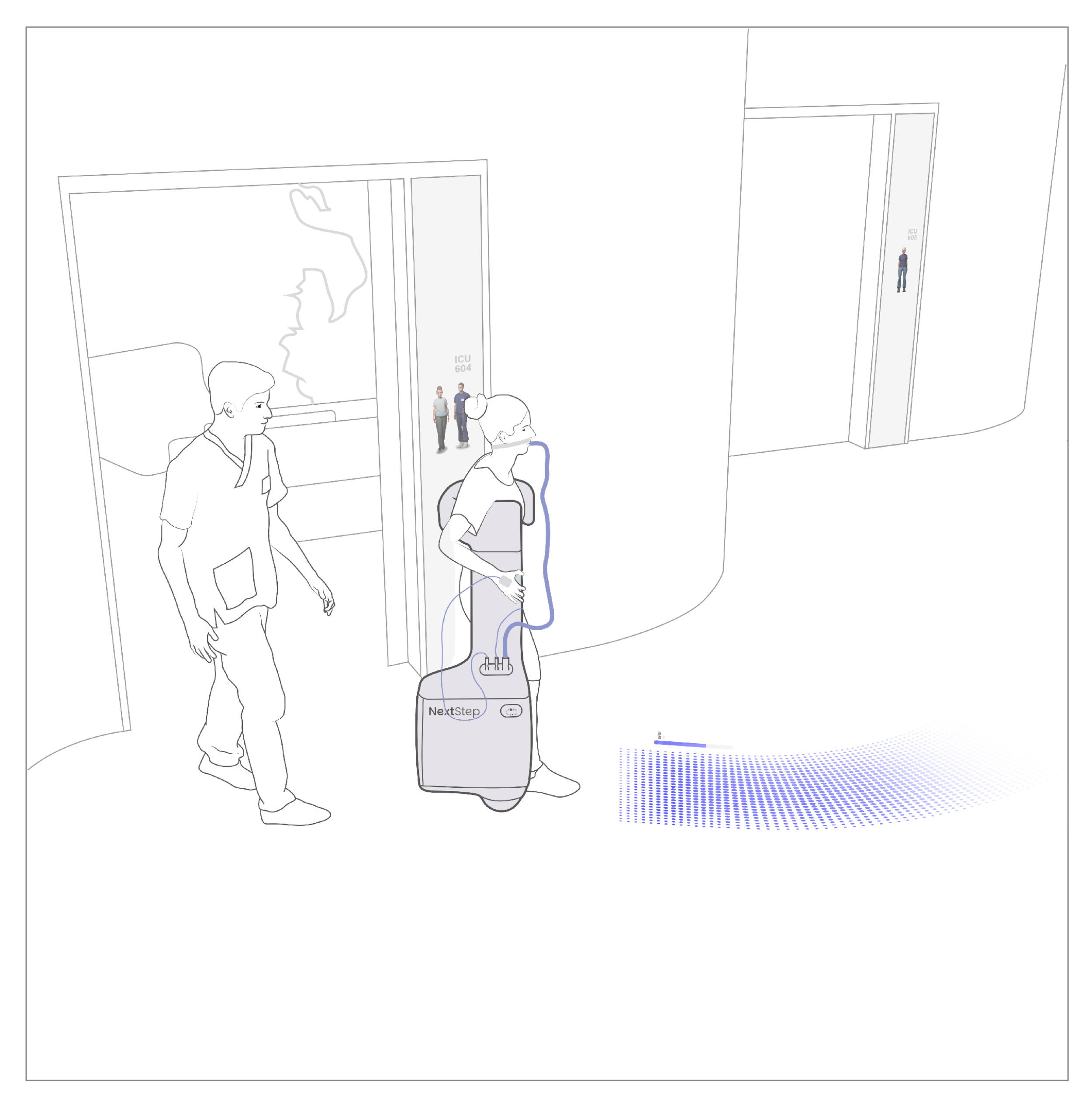
NextStep functions as an adaptive interface to the ICU unit. It continuously monitors vital signs, identifies optimal and safe timeframes for mobilization, and physically supports transitions from sitting to walking. During these sessions, NextStep temporarily takes over life-sustaining systems—allowing movement beyond the limits of stationary ICU infrastructure while maintaining safety and autonomy.
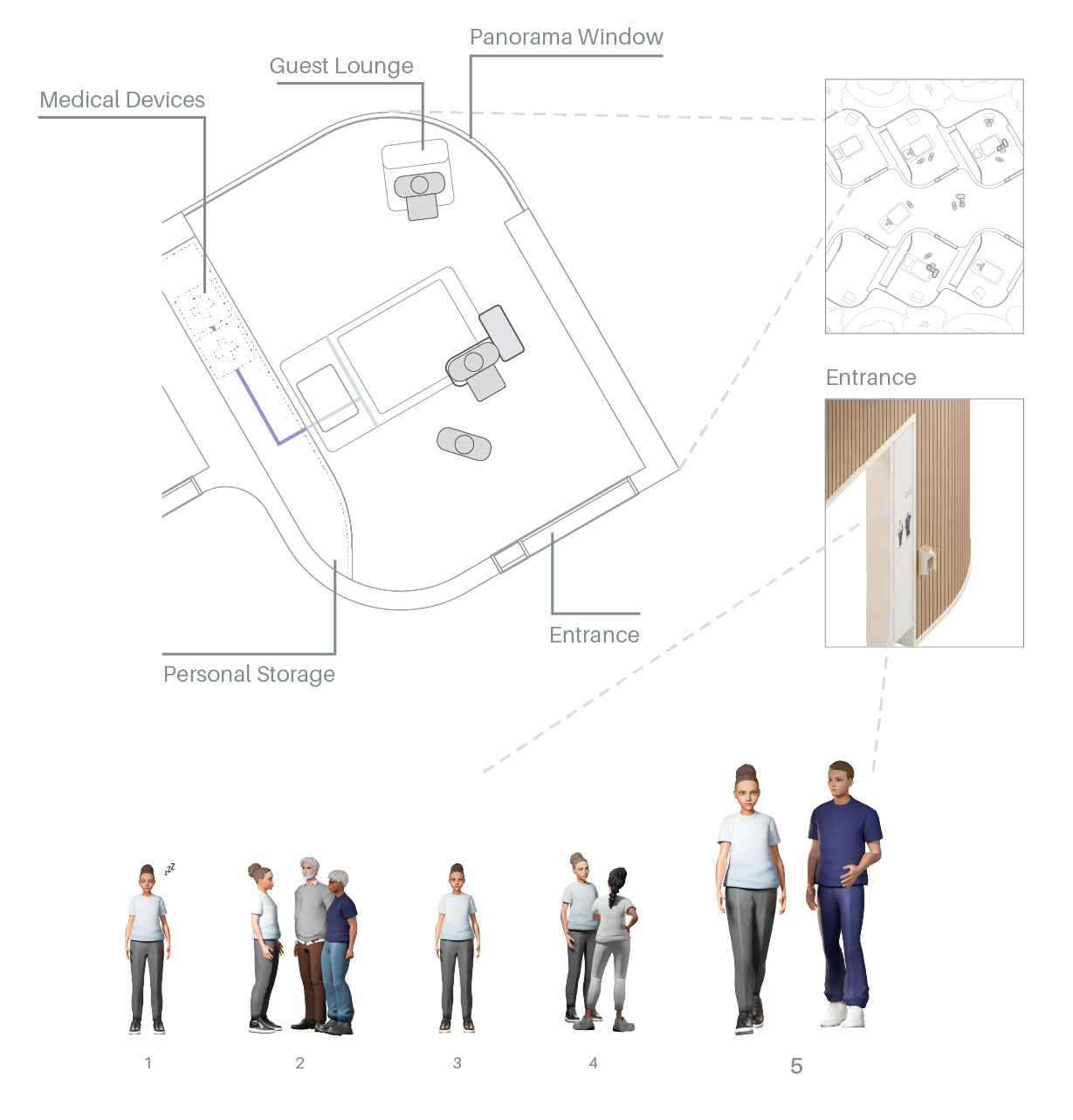
Structure of a Patient-Centered Healing Environment
1 Patient asleep; 2 Relatives visiting; 3 Patient awake; 4 Doctor’s visit; 5 Mobilization
Because critically ill patients often experience a loss of physical control and confidence, the system is designed to actively restore both. NextStep also uses AI-assisted monitoring to reduce alarm fatigue by filtering out non-critical alerts and only notifying staff when action is really needed. During mobilization, dynamic floor projections visualize movement ranges, while built-in stabilization sensors monitor balance and circulatory stability in real time.


Connection ports and adaptive care system modules
NextStep merges intelligent data processing, advanced medical technology, and physical therapy into one coherent system. The result is a new paradigm for intensive care—one that empowers patients, supports clinical staff, and accelerates recovery through targeted, safe, and self-directed mobilization.
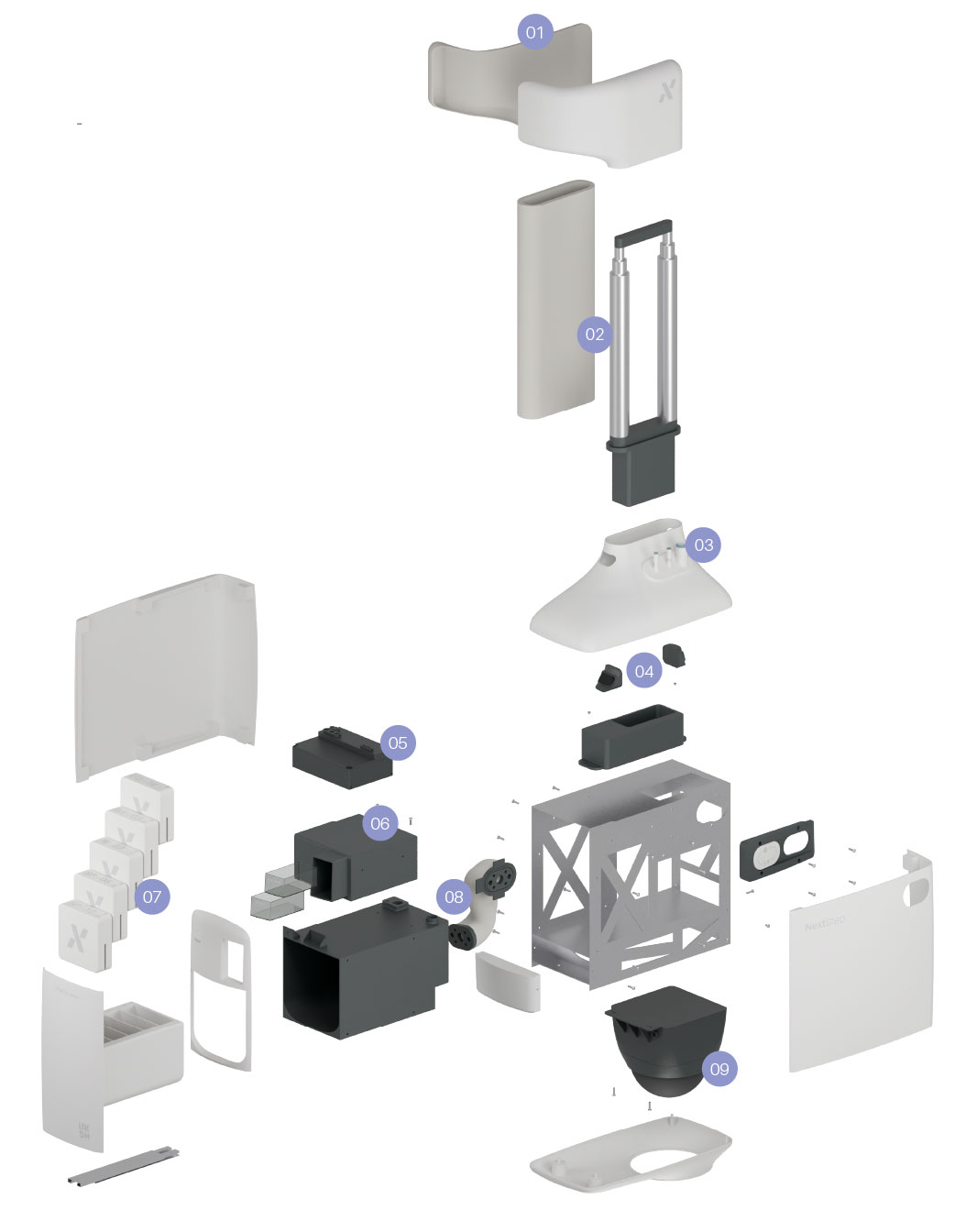
Technical details: 01 Torso Support; 02 Height Adjustment; 03 Patient Interface; 04 Floor/Hologram Projector; 05 CPU and Battery Pack; 06 Ventilator; 07 Adaptive Care System; 08 System Interface; 09 Omnidirectional Weel